THERE is yet another negative report pointed at Jamaica’s premier health-care institution, the Kingston Public Hospital.
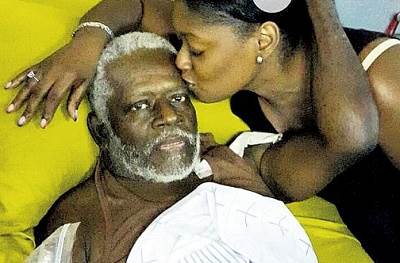
Kenniesha Burrell recounted what she described as a horrific ordeal endured by her father, Michael Burrell, who had gone to the hospital to seek treatment. Michael Burrell eventually died, due to what his daughter claimed was ‘bad treatment’ by KPH staff.
When Burrell contacted the Jamaica Observer, distraught with pain and grief, she said that her ordeal began on December 5, 2014 after a misdiagnosis of acid reflux by private doctors was confirmed at Annotto Bay Hospital to be stage five renal failure. That meant that her father’s kidneys had lost nearly all their ability to work effectively, and eventually dialysis or a kidney transplant would be needed to keep him alive.
“After the doctor told my mommy of the findings, I rushed to my father’s side screaming and crying because this is no news no one wants to hear. When I got there, I saw his mother, my mother and his niece at his bedside and I started to cry all over again.
“He held on to me and started to cry and begged me not to cry because he will be fine and I am only making him weak when I cry. It was the worst feeling ever. I never saw my father cry.
“The feeling of not knowing what will happen seconds, minutes, hours or even days later makes you anxious and weak,” she said.
Burrell further explained that after learning of the seriousness of the condition, the decision was made to transfer her father to KPH, as the doctor at Annotto Bay informed the family that there was no working dialysis machine there, which he would need to stay alive.
At KPH, Burrell said her father was placed on a ward with no beds available and consequently had to sleep in his wheelchair that night.
“The doctor on ward that night asked my father who sent him here, as she was in charge of the ward and if they had called her, they would have known that there were no beds, hence, she would not have taken him,” Burrell said.
She added: “I offered to take a mattress there so he could lay down and rest and I was told that it doesn’t work like that. My dad had to sleep in his chair that night, as sick he was, because of our current health-care system in Jamaica. I begged them to let me stay and I was told in a rude tone by one of the nurses that it was not possible. I left, not because I wanted to leave my dad but because I had to, or face being thrown out by security.”
Burrell said that when she returned in the morning his feet were swollen and he was weak. When she inquired why his feet were not elevated she said she received no response.
“I realise that these nurses are negligent and do not take time out to pay attention to small details,” she said.
After her father received a bed, Burrell said she was informed that based on his condition, they would not be able to feed him. For approximately seven days he consumed nothing but the IV fluid. She said what was to come would leave her in pain as the man who once gave his all for her was now helpless.
“I remember one morning I went to my dad’s bed and saw him bounded tightly to the bed and his lips pasted together with scabs and were very bloody. I asked the nurse and the doctor what was happening; no one could tell me. All I could hear is ‘ask the nurse’. When you ask the nurse, the nurse tell you to ask the doctor. I had to get some water and wipe his lips and clean the bloody area… then a male nurse came and started to assist,” she said.
Burrell continued: “Eventually, when my dad was able to eat, I went to the hospital around 11:00 am and saw his food that came to him from 7:00 am untouched and he was bounded in the bed. I asked the nurse why he hasn’t eaten and she turned to me with an attitude and said ‘mi nah feed him because nuh patient nah spit nuh food pon me’.
“I asked her if he had ever spat on her or any other person in the hospital and her response was ‘you are here now, why you nuh feed him’. I got upset and told her he was my father and I have no problem taking care of him but the fact that he got the warm tea and food from 7:00 am which is not within the visiting hours time and he has not eaten for days, plus he was bound for days, her heart and conscience could not lead her to feed him or even get someone to tidy him off until visiting time and we would do the rest. Some nurses came and tried to assist me while she went and congregated with others, laughing and talking and totally turning her back on the patient.”
Burrell added that after the second day of eating, her father began vomiting and expelled mini clots of blood. She said when she brought it to the attention of the nurse who picked it up in his gloves and rubbed it together, he told her he was not sure what was happening but suggested that her father’s stomach might be irritated since he had not eaten for so long and was now vomiting.
She said he was released days later with his catheter in and started his dialysis privately as the hospital instructed them that there were not a lot of machines at the hospital and even though he was at stage five, he had to be placed on a waiting list with over 4,000 people on it. She, however, gave credit where it was due.
“I must make it clear, though, that he got a few sessions at the hospital while he was there, but he had to seek a private dialysis centre long-term,” she said.
But regardless of his private care, things were still not looking good for Burrell’s dad as his blood count was still low, and his blood pressure and potassium level were high.
“Each time he walked, he would get weak and display fainting signs, and he was bringing up thick clots of blood,” she said. That resulted in her rushing him back to KPH where, after reporting his condition, she was told he had developed an ulcer.
However, according to Burrell, he was subjected to the same treatment as before of not being fed, because of a fear that he would begin vomiting.
Her father, she said, began eating on his own, but was later reprimanded.
“Again, he was there for a couple of days, nothing to eat because they did not want him to vomit. Some days later food and tea was left by his bedside and he drank the tea. I was so happy that he finally could eat again, so I went to ask to talk to the doctor and said that I see he is improving because he started to drink his tea.
“But the doctor turned to a nurse and said ‘how comes bed number so and so drank tea and he is not supposed to eat?’ The nurse went to Daddy on his bed, shouting at him, “yu know yu nuh suppose to drink the tea and yu drink it. Why yu drink it? Anything happen to you a your fault because you are not a child and you knew you were not supposed to drink it,” she recounted.
Burrell said she told the nurse that she was rude and the hospital was negligent. But that drew a caustic response from a nurse’s assistant.
“Yu father a big man, we nah run nuh day care in here, him know him nuffi drink the tea!” Burrell said the nurse wearing a pink and white uniform yelled at her.
“They turned on me, but he begged me not to answer them because when I leave they were going to treat him bad and not pay him any mind,” she said.
As a result, Burrell said an endoscopy to ascertain the cause of the bleeding was put off.
She said that because of his ordeal, her father cried and begged to go home.
“He said to me ‘I want to come out, the treatment nuh good. I am like a boy and a nobody in here’,” she explained.
Moreover, Burrell said she reported the matter to the nurses’ supervisor but she does not know if anything was done as she was not given an update.
However, she said while she tried to remain strong throughout the situation, she was informed that her dad would need Nexium, for heartburn relief, but when she took it, she was shocked at what she saw.
“When I returned in the morning, while giving him a wipe down, I saw a glass, Nexium bottle, a blade, a needle — I’m not sure if it was used or not — and a single glove under his back. When I inquired, they were taken from me and I was told that it was the interns that left them there and that was the end of it. No apologies, no alarm, no concerns, no nothing because obviously this was not new, apparently this is an everyday thing,” she said.
Not long after, Burrell said, a change of events unfolded as her father’s health deteriorated further as his blood count started to fall drastically and he needed blood. It was not long after that, Burrell said, he had passed out at the hospital and when she was informed and rushed to his side she found him confused, weak and bleeding uncontrollably into his adult diapers.
“I cried and begged God to save him and give him a chance to live to see the new year. The doctors on that particular ward assisted him a lot, they were patient and really went beyond the call of duty for him,” she said.
She stated that one doctor got up and gave blood for him, for which she was very grateful and he was rushed to do an operation to stop the bleeding.
But she said after the operation he was released with no medication for pain or infection, no prescription. Neither was she advised how to care for such a patient who was facing other medical problems.
“Despite my many queries forwarded to the nurses, I was told I had to speak to the doctors and all were in theatre operating. So I had to leave and come back another day to see his doctors. About two days later, while at home, he started to complain about his stomach feeling weird and full and the top part seemed not to be healing. His tummy was hard and puffy and he said he felt like he wanted to burp or pass gas and it was not happening. The next morning, he got up to use the bathroom and started feeling weak again, I took him back to the bathroom and he again started to pass coffee-brown blood,” she said.
Burrell said when she took her father back to the hospital she was told it was not an emergency and she had to go through the normal procedure and wait at the front to see the nurse, the doctor and then be transferred to the emergency area to be registered, which resulted in him being admitted for the third time in one month.
However, she said after he spent one week on the ward, she received no update on him, and was just informed to take the medication she had bought for them to continue his treatment.
“I kept asking them what they were going to do about the discomfort and I got no response. He got needles and drip a few times and after that he was basically just there waiting to die,” she said.
On the morning of January 5, 2015, Burrell said her father phoned her to say he was feeling dizzy and that he was calling the nurses but no one came to him. When she inquired, she was again met with disdain.
“I called the hospital and explained to a nurse what was happening and another nurse in the background said ‘mi nah go nuh weh to him, sometimes them nuh want nothing, Them only just want to see you walk past’. I said to the nurse on the phone, ‘I heard everything she said and I truly can’t believe this is the situation my father is in’. I went to see him during visiting hours at 11:25 am and he told me he was passing blood and that he almost fainted in the bathroom the night before but a patient assisted him to a wheelchair. He went further and said he called the nurses to assist him to the bathroom and they didn’t come and when he almost fainted patients were calling the nurses and they didn’t come.
“He told me a patient pushed his wheelchair to the bed and helped him back on the bed. I spoke to the doctor, he told me he is not aware of those events and as far as he knows dad is not loosing blood and he is positive,” she said.
But regardless of the doctor’s assurance, she said her father’s blood count had drastically fallen.
“My father went into the hospital with about eight point something blood count and when the doctor came to me he told me my father’s blood count was at three, which is not good. I said to him ‘look from when I am coming and asking for an update, nurse send me to doctors, doctors send me back to nurses. I know he never lost all that blood overnight’. He said I needed to get as much people as I can to give blood and so I blasted on my WhatsApp at 11:39 am to all my friends that my dad needs blood and I am asking all to assist. I got a lot of persons willing to give blood and I called my daddy 10 minutes later, about eight times, to tell him that all will be well and to leave all the worrying to me. He didn’t answer any of my calls,” she said.
It was on the ninth call that Burrell learned her father had passed as someone answered the phone and gave her the terrible news.
“He said by the time I left he started to bring up blood through his nostrils and mouth and they called the nurse and no one came until it was too late,” she said. “I went to the hospital and I told them what I was told and asked if it was true. The nurse was on her phone and said ‘please have a seat, the doctor will soon be with you’. I waited for 43 minutes and no one came to me. I got up and started to ask if this is the way they deal with relatives at a time like this.
“I said, first to note, while I was on the road trying to get blood for my dad, he died and no one called to tell me to come in or nothing. The nurse said ‘that’s not how it works, they have to fill out paperwork first, then the doctor will call in the relatives’.
“She went further to say that the person who answered the phone should be discharged because ‘him too fass and nuff’. I said it was a relative who saw everything and answered and that’s your response to me, a human being who just lost her dad. They all ignored me, continued laughing and talking on their phones showing each other whatever it was on the phone.”
Burrell described her experience as painful and one she will never forget. She is adamant that there should be no repeat of her father’s ordeal.
“I’m not saying he wouldn’t have died. It’s how it was dealt with. What if they had got up? Probably he would have been alive today. When will this ever stop? What is it that we’re doing for patient care?
“I was crushed and destroyed and I know for a fact if the nurses were more alert, not negligent, and really concerned about patients’ health he might still be alive. I need answers as I cannot let it go. I cry every night and I do not know what to think and what to do.
“The day my father died, I told my friends that we should set up a dialysis centre in the parish we are from because we can help people. I cannot fulfil that dream right now but for sure his name and memories will live in all I do, ” she said.
Burrell described her father as a man who was not financially well off, but he showed his family love.
“I remember being sick as a child and I was admitted to the hospital in Port Maria and he walked from Annotto Bay to Port Maria to be by my side,” she said.
“I am so heartbroken and I am finally locking myself away to cry as I feel like I can’t be strong anymore, but I have to because I can’t let him down.
“It pained me to see him suffer like that and not being able to call me ‘shubby dubby’. I just want my father back and I have prayed and prayed and I know God knows,” Burrell said.
When the Sunday Observer contacted KPH’s Senior Medical Officer Dr Natalie Whylie, she said that while she was not aware of the details surrounding the incident the hospital has mechanisms in place to manage patient complaints.
“The complaints can be made to the nursing staff and the nursing staff has levels of supervision. There are always doctors there and the team of doctors are headed by consultants. We have a patient affairs director whose job is to take complaints and to investigate — to see what is happening, and there is the director of nursing services and myself, the senior medical officer,” she said.
Dr Whylie asked to be provided with the information, patient’s name and what happened in order to immediately initiate an investigation.
As for Burrell and her relatives, Dr Whylie requested that they come in and speak to her for her to hear their concerns.
“Usually, what we do in that situation is have the matron of the hospital and the deputy matron, along with the patient affairs manager meet, hear the complaints and initiate an investigation and depending on the result of the investigation, we initiate action as well. We’re constantly in the business of auditing patient care and hearing where the gaps are so we can improve patient care at KPH,” she said.
Moreover, she expressed concern at the family’s well-being and said that a further step the hospital will have to make is to assess how to help Burrell and her family through their pain.
“It is a case where someone has lost a loved one and we have to look at what is happening to our patients. Give us an opportunity to deal with it,” Dr Whylie said.

Shameful. If some a dem deh nurse fi come a foreign come wuk dem would a haffi deh pon dem peas and cue. They really have no respect fi poor people. The government fi dem.
Shameful. If some a dem deh nurse fi come a foreign come wuk dem would a haffi deh pon dem peas and cue. They really have no respect fi poor people. The government fi fire dem.
So sorry to hear of this young lady loss. I know what she is going through. In 2003 when my husband died and we took him to Jamaica for burial. 3 days after the funeral I was admitted in University Hospital due to gall stones. They wanted to remove them to which I refused and told the Drs that I would seek medical care back in the United States. On day 2 of my stay a lady in my ward directly across from me, who is allergic to to penicillin and sulphur medication clearly indicated on her chart. Was given penicillin and had a severe allergic reaction. Her tongue became swollen, her eyelids peeled among other reactions. If one of her daughters not shown up late that night I shudder to think what would have happened. When the very effeminate half chiney dr finally showed up the morning. After being approached by the lady 3 daughters, he laughed and said this is nothing worse than this happens. Then to add insult to injury the daughters were told the medication to reverse the reaction was not available in the hospital pharmacy. They had to spend thousands to rectify the damage done by the hospital. I informed that chiney dr that if this happened in America there would be a major law suit, to which he laughed and informed did a no America. I promptly called my family and voluntarily discharged myself. Jamaican’s health care system is in shambles. If you can afford to go to the Thwaites division your good but if your poor, woe be unto you. Portia need to have spent the money she spent to impress Barak on her failing health care system
I cried while reading this, I don’t understand why some of these nurses go into a profession that deals greatly with compassion, patience and care which most of them don’t exude and they are downright unprofessionals. Mi a tell u seh being poor outta Jamaica deh is s crime, but nuff a den fassy hole nurses deh fi guh find a different profession do like guh sell a market or inna bar…smh
I cried while reading this, I don’t understand why some of these nurses go into a profession that deals greatly with compassion, patience and care which most of them don’t exude and they are downright unprofessionals. Mi a tell u seh being poor outta Jamaica deh is s crime, but nuff a den fassy hole nurses deh fi guh find a different profession do like guh sell a market or inna bar…smh
What wickedness, why are these people in health care if they are not there to help, this is just unbelievable!! May the good lord have mercy on those that have to depend on the healthcare system in JA. U going to tell me that you have so many occurrences of neglect, disregard and brutal behavior towards patients and still nothing? My God man, Lord I ask for your mercy for my fellow men:(
I was a registered nurse in Jamaica however migrated to work somewhere else. Every word in this report is true. I have had the opportunity of taking patients from my hospital to KPH that we were not able to manage and I also visited friends who were admitted there. The treatment that the patients get is atrocious!!! Nurses and doctors would be on their phones or just chatting at the nurses’ station. DEATH and suffering don’t mean anything to those staff anymore. We had a patient who was admitted there and when he was sent back to us, his anus was stuffed with gauze because he had diarrhoea. What a wicked act!!!!!
They blame the treatment on poor staffing but I think some of us are just heartless and went into the profession for the wrong reason/s. Dont we have a conscience? When I see my patients I see myself or a family member, so empathy will always be at the forefront when I care for them.
You know what is ironic when we go abroad we are the best nurses and we treat our own people like ‘dirt’. My colleagues let us do better and remember the nursing oathe that we all pledged to!!!!
This read like something out of a horror movie. I cannot imagine that this happened in real life. Living nightmare and a national disgrace!