How beans, unripe banana, rice promote good health
To many people, starch is a form of carbohydrate that causes weight gain and shoots blood pressure up. But surprisingly, experts say consumers of a diet high in carbohydrate can reap many health benefits from something called resistant starch, which is a “good carbohydrate.”
Well, experts have found that consuming foods rich in resistant starch such as bananas and potatoes may make healthier by decreasing appetite and short-term food intake, improving digestive tract or gut health, reducing bad cholesterol and keeping the blood sugar under control.
All carbohydrates are not the same. Like its name implies, resistant starch escapes digestion in the small intestine and makes its way to the large bowel, where it is slowly fermented and broken down by good bacteria.
Fermentation creates short-chain fatty acids, compounds that feed gut (digestive tract) bacteria, fuel colon cells, prevent the growth of harmful bacteria, fortify the intestinal lining and help regulate immune function.
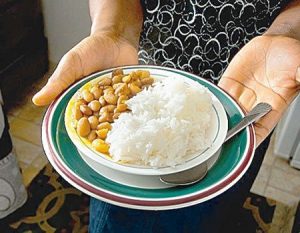
Good sources of resistant starch include white beans, chickpeas, lentils, green peas, cashews, unripe bananas, plantain, whole-meal rye bread, barley and raw oats.
Also, rice, potato, yam and pasta that have been cooked and cooled are sources of resistant starch. Cooling cooked starches changes their structure, making them resistant to digestion in the small intestine.
In fact, resistant starchy foods are bulky. It takes up space in the digestive system. A good example is eating boiled potatoes that fills up the stomach, wanting no other food.
Basically, the intestines are home to trillions and trillions of microbes, the vast majority of them residing in the large intestine. Collectively, these bacteria, yeasts and fungi constitute what’s called the microbiota.
The microbes in the digestive tract extracts energy and nutrients from fibre, synthesises certain vitamins, activates disease-fighting phytochemicals, regulates immune function and protects the lining of the tract.
Without a steady supply of resistant starch, the healthy microbes that reside in the digestive tract can die off, increasing the load of disease-causing bacteria. Running down the good microbes may also increase the risk of allergies, type 2 diabetes, obesity and inflammatory bowel disease.
Growing evidence suggests this microbial community also plays a role in inflammatory bowel disease, mental health, weight control and, even food cravings.
Each person’s digestive tract is unique and always changing. Genetics, antibiotic use, hygiene, stress and illness can shape its microbial community.
All the same, diet is considered the most powerful tool that can alter the composition and activity of microbes in the digestive tract. A western-style diet because it is high in animal protein, saturated fat and refined carbohydrates but low in fibre has been linked to a loss of good bacteria in the digestive tract.
By not eating enough resistant starch, good bacteria can feed on other things, which can damage the digestive tract. The bacteria in the digestive tract of mice starved of fermentable fibre have been shown to feed on its lining, making it thinner and more vulnerable to infection-causing bacteria.
Resistant starch is the focus of a 2015 study in the journal Nutrition Bulletin. The researchers from the British Nutrition Foundation and University College, Dublin, in Ireland provides fresh evidence that resistant starch may help control blood sugar, enhance satiety and support digestive tract health.
Stacey Lockyer, Nutrition Scientist at British Nutrition Foundation stated “We know that adequate fibre intake – at least 30 grammes per day – is important for achieving a healthy, balanced diet, which reduces the risk of developing a range of chronic diseases.”
For their research, the researchers analysed the published literature and found a variety of different reasons to incorporate this form of starch in daily diet.
Some published studies also stated that consumption of resistant starch can reduce the adverse health effects of consuming a lot of red meat on colorectal cancer risk. But, the researchers affirmed more research is needed to determine these potential health claims.
Intake of whole grain varieties of resistant starchy foods instead of white versions of these foods is beneficial for achieving a good health, they said.
“Whilst findings support positive effects on some markers, further research is needed in most areas to establish whether consuming resistant starch can confer significant benefits that are relevant to the general population; however this is definitely an exciting area of nutritional research for the future,” Lockyer concluded.
Previously, researchers at the University of Florida had said that eating between 14 and 42 grammes of almonds or almond butter daily can help displace empty calories, and improve friendly bacteria composition in the digestive tract.
The study found that a “moderate” amount of almonds significantly improved overall diet quality and modulate intestinal bacteria composition in participants of the study.
Although no specific changes in immune markers were observed, almond consumption did result in detectable changes in microbe concentration of the gut, which may have a variety of digestive and immune health benefits.
